The Fitzpatrick Factor
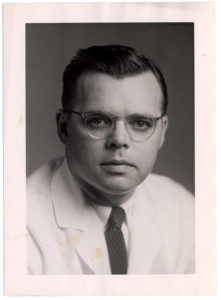 The father of modern academic dermatology and a giant in the advancement of clinical and investigative dermatology, Dr. Thomas B. Fitzpatrick was born in Madison, Wisconsin on December 19, 1919. Fitzpatrick went on to serve nearly 30 years as the chairman of the Department of Dermatology at Harvard Medical School and Chief of the Dermatology Service at Massachusetts General Hospital. His contributions to the field were tremendous: his renowned multi-author book Dermatology in General Medicine is used to this day; he was a passionate teacher and trainer, and his discoveries and research led to therapies that combat psoriasis and forms of skin cancer. His innovative pursuits led to more effective treatment of skin diseases.
The father of modern academic dermatology and a giant in the advancement of clinical and investigative dermatology, Dr. Thomas B. Fitzpatrick was born in Madison, Wisconsin on December 19, 1919. Fitzpatrick went on to serve nearly 30 years as the chairman of the Department of Dermatology at Harvard Medical School and Chief of the Dermatology Service at Massachusetts General Hospital. His contributions to the field were tremendous: his renowned multi-author book Dermatology in General Medicine is used to this day; he was a passionate teacher and trainer, and his discoveries and research led to therapies that combat psoriasis and forms of skin cancer. His innovative pursuits led to more effective treatment of skin diseases.
Dr. Fitzpatrick received his bachelor’s degree from the University of Wisconsin and went on to graduate with an MD from Harvard Medical School. He interned at Boston City Hospital and it was there that he recognized a significant imbalance of priority between dermatology and other medical specialties. It became Fitzpatrick’s quest to remedy that imbalance. At the University of Minnesota, where he earned his PhD in Pathology, Fitzpatrick met fellow MD and PhD Adam Lerner, with whom he conducted substantial research on skin pigmentation that led to ultraviolet light therapies to treat psoriasis and other severe skin diseases. Fitzpatrick continued advancing his knowledge and took up dermatology training at the University of Michigan and the Mayo Clinic. At 32, he was recruited by the University of Oregon to be Professor and Chair of Dermatology. Harvard would invite him only seven years later to assume the chair of the Dermatology Department. At 39, he became the youngest professor and chair at Harvard.
Among his scientific contributions are the Fitzpatrick Scale, developed in 1975 and used to this day, a numerical classification of skin color and how UV rays affect different skin tones. This discovery led to his quantitative research of the effectiveness of sunscreen. He also helped establish clinical criteria that improved the diagnosis of malignant melanoma, and his research on the epidermal melanin unit fundamentally changed modern dermatology’s understanding of skin pigmentation. Fitzpatrick passed away in Massachusetts in 2003 at age 83. – Michelle Meagher
Skin Cancer Causes
Like all cancers, skin cancer is caused by cell mutations that grow uncontrollably to form a mass of cancer cells. Because the skin is comprised of three main types of cells, there are three primary forms of skin cancer with different treatment methods: basal cell carcinoma, squamous cell carcinoma (SCC), and melanoma, the most virulent, yet rare form of skin cancer.
Basal cell carcinoma (BCC) is the most common form of skin cancer, according to the Irish Cancer Society. Basal cells are located at the base of the outer layer of skin, and their primary function is to produce new skin cells. If left untreated, BCC will eventually form what is known as a “rodent ulcer,” a pearly or waxy bump that usually occurs in the most sun-exposed areas of the body, i.e. the face, ears, or neck. It can also manifest as a flat, flesh-colored or brown scar-like lesion.
Squamous cell carcinoma (SCC) is the second most common form of skin cancer in Ireland. It forms in the squamous cells, which are the top-most layer of skin and usually manifests on frequently sun-exposed areas like the face, ears, hands, and arms, generally taking one of two forms: a firm, raised red lump, or, a flat, crusted and scaly lesion. Because both BCC and SCC are located in the outer layers of skin cells, which have fewer blood vessels, they are unlikely to spread to other parts of the body – unlike melanoma.
Melanoma is the most severe form of skin cancer and grows in melanin-producing cells, which are responsible for giving the skin its pigment. Because melanin is produced in other tissues, like the eyes and intestines, melanoma can occur anywhere on the body and is not necessarily restricted to sun-exposed areas of the skin – sometimes occurring under the fingernails or toenails, on the palms of the hands, and on the soles of the feet. If melanoma is not removed, the enlarged cells can grow deeper into the skin and spread via blood vessels to other areas of the body, complicating treatment options.
Skin cancer is an especially prevalent issue in Ireland, where cases have more than doubled in the past 20 years, according to the Belfast Telegraph in June. Moreover, between 1998 and 2008, according to a 2010 National Cancer Registry of Ireland report, melanoma rates in Ireland have increased 91%, from 393 diagnosed cases to 752 in 2008. The same report documented that Ireland has among the highest national rates of skin cancer: one in eight Irish men and one in ten Irish women will be diagnosed by the age of 74. In comparison, in the United States, one in five people will be diagnosed with skin cancer during their lifetime. According to the Skin Cancer Foundation, since 2000 melanoma has been the only one of the seven most common cancers whose incidence increased rather than decreased in the U.S.. Melanoma rates are steadily rising at a rate of 1.9 percent each year, and in 2013 alone, the American Cancer Society estimates that 76,690 new cases of invasive melanoma will be diagnosed.
One of biggest misconceptions about melanoma is that it isn’t a concern for young people. “Melanoma is the second most common cancer in young people ages 15–29. It is a myth that melanoma is an older person’s disease,” said Deb Girard, executive director of the Melanoma Foundation New England. Young people must get skin checks too, especially if they have any risk factors.
Risk Factors
There are many risk factors for developing any type of skin cancer, though almost all of them have to do with the sun and skin tone. They include:
• Having fair skin: Because melanin protects the skin from harmful UV radiation, people with darker skin tend to have lower rates of skin cancer, while people with fair skin, especially people with blond or red hair and light eyes, are at a greater risk.
• Blistering sunburns: Having one or more sunburns that blistered, especially as a child, increases your risk of skin cancer. Sunburns in general also increase your risk.
• Excessive, unprotected exposure to sun (including regular tanning bed use).
• Having atypical or numerous moles (over 100) indicates a greater risk for mel-anoma, which can begin as a benign mole.
• Having a family history or personal history with skin cancer.
Because skin cancer can take 20–30 years to develop fully, it is important to recognize these risk factors and maintain a close watch on any skin abnormalities that develop, especially moles.
Symptoms
As forms of skin cancer vary, so do the symptoms. They can include:
• A small lump
• Flat, red spot
• Firm, red lump
• A lump or spot that is tender to touch
• An ulcer that will not heal
• A lump with a scaly or horny top
• Rough, scaly patches
For melanoma specifically, you can follow the ABCDE checklist:
A. Asymmetry: melanomas have two distinct halves and are not symmetrical if cut in half.
B. Border: as opposed to a regular mole, melanomas have rough and ragged edges that are clearly defined.
C. Color: melanomas have two or more colors, light brown to black, and may be an entirely different color from other moles.
D. Diameter: melanomas are larger than 1/4 inch in diameter (6mm).
E. Evolution: a mole that changes in shape, size, or color, whether over time or rapidly, is likely melanoma.
Importantly, while not all skin abnormalities are cancerous, some cancerous skin conditions may not follow these guidelines exactly, so it is important to consult a doctor if anything concerns you.
Treatment
Fortunately, the majority of skin cancers are benign and treatable. Up to 97% of melanoma cases are treatable if diagnosed early enough. Treatments vary depending on a number of factors, including location, size, type of cancer, its depth, or the patient’s age, but the most common form is excisional surgery, where the cancer is removed along with a small amount of normal skin around the growth. Other treatments may include:
• Cryotherapy, or freezing with liquid nitrogen.
• Laser therapy
• Radiation treatment if surgery is not an option.
• Chemotherapy in the form of a cream that is applied directly to the cancer.
• Biological therapy, or immunotherapy, consists of training the body’s own immune system to fight the cancer cells.
• Photodynamic therapy that uses a beam of light in conjunction with light-sensitive drugs to destroy superficial cancers.
Prevention
Nearly all skin cancers are avoidable. You can significantly lower your risk by:
• Wearing at least SPF 15 sunscreen year-round and reapplying every two hours, even when it’s cloudy. A golfball-sized drop is recommended. (See the new sunscreen regulations and a buying guide below)
• Avoiding the sun when it is the strongest, in the middle of the day.
• Avoiding tanning beds
• Wearing protective clothing, including sunglasses and a broad-brimmed hat if you expect to be in the sun for extended periods of time.
Most importantly, frequently check your skin, including areas not usually exposed to the sun, for changes in existing freckles, moles, and bumps, or for new growths, and report any changes to your dermatologist. For those who need a little help resisting the allure of tanning, the Melanoma Foundation of New England offers a No Tanning Pledge – with different variations for high-schoolers, college students and the general public – in conjunction with its Your Skin is In initative. Visit mfne.org/prevent-melanoma for more information.
New Sunscreen Regulations and Tips
This summer, the FDA introduced new sunscreen labeling regulations. Here’s your quick guide to understanding what they mean and what to look for:
• “Broad Spectrum Protection” on a bottle will mean that the sunscreen protects against the two types of ultraviolet light the sun produces, UVA and UVB. Until recently, most sunscreens only protected against UVB rays, which directly cause sunburn. However, experts now believe that UVA rays, while not sunburn-causing, contribute to the risk for skin cancer, especially melanoma.
• Products can no longer claim to be “waterproof,” only “water resistant,” and must include a time limit of either 40 or 80 minutes before the protection becomes ineffective and reapplication is necessary.
• All sunscreens with an SPF under 15 must carry a warning label saying they do not protect against skin cancer.
• Even though sunscreens with SPFs greater than 50 are still on the market, the FDA is considering banning them because they are not proven to provide greater or longer protection, despite the public perception of their effectiveness.
• Endorsements and private approval ratings are still allowed, but consumers should be weary. According to the New York Times, the Skin Cancer Foundation gives a “seal of recommendation” to sunscreens only after the company has given $10,000 to become a member.
Buying Guide
• Use SPF 15-50 depending on your skin type. Lower SPFs are ineffective and higher SPFs are unnecessary.
• Only buy sunscreens labeled “Broad Spectrum Protection.”
• Avoid sprays, which usually don’t cover all the surface area of the skin and can be accidentally inhaled. The FDA has banned powder sunscreens and requested more information on sunscreen sprays.
• The Environmental Working Group recommends purchasing products with zinc oxide or titanium dioxide as active ingredients. These compounds do not degrade with exposure to light and are usually found in heavier, oily, opaque “sunblocks.” (Think lifeguard with a white nose.)
• Use fragrance-free sunscreens, which avoid unnecessary chemicals and potential allergens. – Adam Farley


Leave a Reply